Pr Cédric BARREY
Service de neurochirurgie – chirurgie du rachis et de la moëlle épinière
Au sein de l’hôpital neurologique Pierre Wertheimer qui regroupe les équipes et expertises les plus en pointe en matière de neurologie et neurochirurgie, le service prend en charge l’ensemble des pathologies du rachis et de la moelle épinière de l’adulte.


Projet
Les projets de recherche fondamentale
Les projets de recherche fondamentale sont menés dans 2 domaines particuliers :
- La biomécanique
- Les substituts osseux
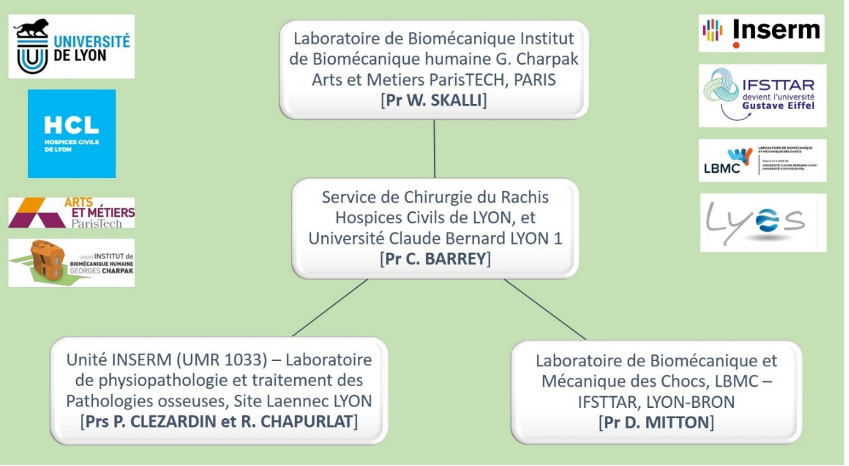
Ces projets et travaux de recherche sont développés + particulièrement en partenariat avec 3 laboratoires de recherche (voir schéma ci-dessous) :
- Le laboratoire de biomécanique des Arts et Métiers de Paris « Arts et Métiers Paris Tech », Institut de Biomécanique Humaine G. Charpak, dirigé par le Pr W. SKALLI
- Le laboratoire de biomécanique et mécanique des chocs, LBMC, Pr D. MITTON, Lyon-BRON (IFSTTAR)
- Le laboratoire INSERM UMR1033 – Pathophysiology, Diagnosis and Treatments of Bone Diseases – LYOS, Site Laennec (Pr P. Clezardin, Pr JP. ROUX, Pr R. CHAPURLAT), spécialisé dans le domaine des greffes osseuses.
Il s’agit plus précisément de :
- développer un modèle prédictif des complications mécaniques de la chirurgie du Rachis – Projet SKAIROS – avec Arts et Metiers Paristech
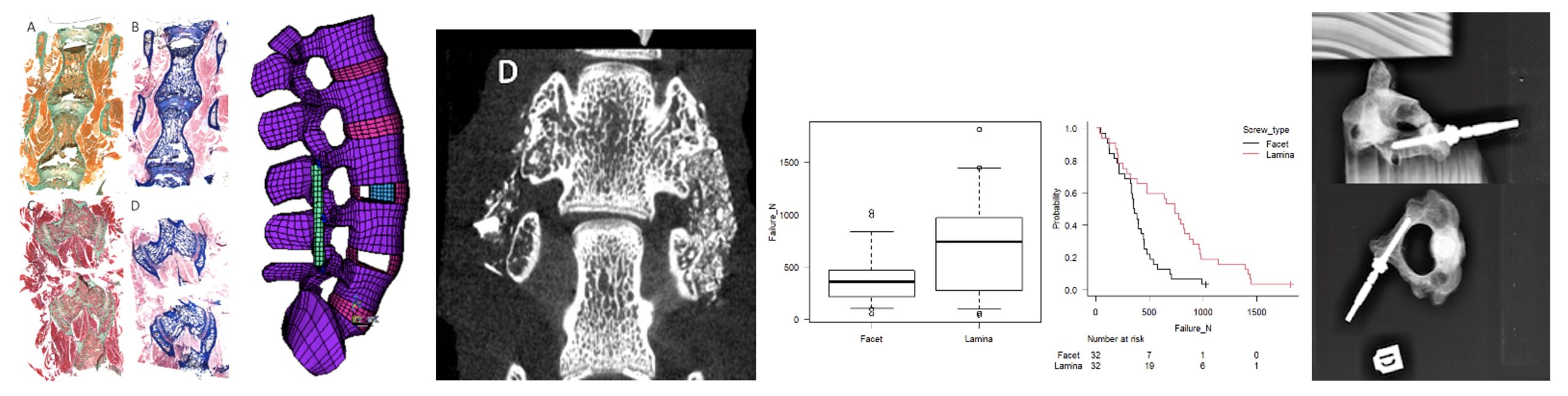
- évaluer de nouveaux implants rachidiens (prothèse discale cervicale, instrumentation rachidienne postérieure) et/ou de nouvelles techniques chirurgicales. Master II en cours du Dr A. MEYNARD, CCA en nov 2021, sur un protocole d’évaluation In Vitro des vissages de C2 – avec LBMC/IFSTTAR
- Projet MEKANOS : créer un modèle prédictif de la faillite mécanique d’une vertèbre métastatique – expérimentations In Vitro et modélisation numérique – avec LYOS et LBMC/IFSTTAR
- projet de Master de Théo BROUSSOLE sur le Bioverre en lien avec l’Ecole Veto de Lyon, l’Ecole de Chirurgie (Rockefeller) et l’Unité INSERM (Pr R Chapurlat). Etude In Vivo pré-clinique chez l’animal sur l’efficacité du Bioverre pour la consolidation osseuse. Partenaire industriel : NORAKER, Villeurbanne – avec LYOS.
- Projet de développement d’une cage bio-résorbable 3D (pour les arthrodèses rachidiennes lombaires et cervicales) – partenaire industriel NORAKER™. Projet ayant obtenu un financement par la Région Rhône-Alpes-Auvergne.
Principaux projets de recherche clinique
- PHRC (investigateur principal : Pr C. Barrey) pour l’étude de la correction des déformations sagittales du rachis à l’aide d’une tige pré-cintrée personnalisée. Financement obtenu à 100%. Premiers recrutements débutés en avril 2016. Etude sur 4 ans (deux ans de recrutement, deux ans de suivis).
Etude prospective multicentrique randomisée ++ Analyse des résultats en cours. - Projets de recherche clinique avec partenaires industriels
- Intérêt des bandes sous-lamaires pour la stabilisation du rachis (société Implanet™)
- Intérêt des tiges sur mesure – techniques d’intelligence artificielle (AI) – modèles prédictifs – chirurgie personnalisée – planification de la correction chirurgicale (société Médicréa-Medtronic™)
- Intérêt des cages polymère-titanium pour la fusion vertébrale – rachis cervical et lombaire (Société Global’S™)
- Table ronde SFCR 2022 : Etude prospective multicentrique sur le traitement de la scoliose de l’adulte analyse comparative : traitement par corset versus traitement chirurgical
- Etablissement d’un score IRM de sévérité de la myélopathie cervicarthrosique (1ère cause de compression médullaire de l’adulte). Sujet de thèse d’A. MORGADO.
- Etude prospective : Evaluation de la technique « lateral PLIF » (>110 patients). Dr G. CAPO.
- Etude prospective : Evaluation d’une pâte du bioverre dans les greffes osseuses lombo-sacrées (>40 patients). Dr A. MEYNARD
Publications
1. Clipping Test of a Radiculomedullary Artery During Resection of a Dorsal Spinal Meningioma
Barrey CY, Baassiri W, Vandenbulcke A
World Neurosurg (2022) — Résumé
Arterial supply of the spinal cord is derived from the anterior spinal artery (ASA) and 2 posterior spinal arteries. In the thoracic spine, a few segmental arteries give origins to radiculomedullary arteries (RMAs) that supply the ASA and posterior spinal arteries.1 In the lower thoracic spine, the supply is provided by the Adamkiewicz artery. Spinal meningiomas may be embedded and/or supplied by the RMA, which may be sacrificed to obtain complete resection. Safety of the thoracic RMA occlusion is controversial,2 especially if the Adamkiewicz artery is involved.3 Somatosensory evoked potentials (SSEPs) and motor evoked potentials (MEP) are proposed to detect spinal cord ischemia.4 The RMA supplies the anterior spinal cord, and MEPs seem to be more sensitive than SSEPs to test RMA occlusion.2 SSEP and MEP monitoring during temporary occlusion has been described and significantly changes at 2 and 7 minutes of occlusion.5-8 Safe occlusion with unchanged MEPs after 10-minute temporary occlusion of 32 segmental arteries was reported by Salame et al.9 We intraoperatively discovered an anterior T10 RMA supplying the adjacent meningioma (Video 1). We temporary clipped the artery for 8 minutes. MEPs were recorded before clipping and every 2 minutes. No changes were observed, and the artery was sacrificed. RMA or segmental artery ligature may be required and is frequently performed in deformity, oncologic, and vascular spine surgery. The clipping test with MEP monitoring is a useful and simple intraoperative tool to identify the critical afferents of the ASA. It doesn’t require planification or supplementary materials. Further study might be performed to validate the technique.
2. Cysts associated with intramedullary ependymomas of the spinal cord: clinical, MRI and oncological features.
Dauleac C, Messerer R, Obadia-Andre N, Afathi M, Barrey CY
J Neurooncol (2019) — Résumé
Purpose: Few published articles have explicitly focused on cysts associated with intramedullary (IM) ependymomas. The objective was to assess the clinical, MRI, and oncological results of patients operated for an IM ependymoma associated with a cystic portion. Methods: During the study period, 23 IM tumors resected were cystic ependymomas. The modified McCormick scale was used to assess the neurological function of patients. The diagnosis of cystic spinal cord tumor was made on preoperative MRI. Results: Two types of cysts were identified according to their location: either intra-tumoral cysts (ITC) or satellite cysts (SC). ITC (52.2%) were more frequent than SC (21.7%), but 26.1% of patients presented both. ITC were enhanced by gadolinium while SC were not. The solid portion of ependymomas with ITC was significantly larger than the one of ependymomas with SC (p = 0.002). The mean time to the first occurrence of symptoms was significantly shorter in patients with neurological deficit than those without a deficit (p = 0.04). GTR was achieved in 78.2% of cases. Complete excision of the cysts was easier when they were larger (p = 0.006). Sixty percent of cysts disappear postoperatively. Persistence of satellite cysts despite GTR of the tumor, and with no recurrence of a tumor on the post-operative MRI, was observed for 3 patients. Conclusion: ITC and SC are different in location, volume, gadolinium enhancement. Their surgical management is different since ITC are resected while SC are drained. Cystic recurrence and/or persistence are not synonymous with tumor recurrence.
3. Chronic low back pain: Relevance of a new classification based on the injury pattern
Barrey CY, Le Huec JC; French Society for Spine Surgery.
Orthop Traumatol Surg Res (2019) — Résumé
Background: The objectives of this study were to define the role for surgery in the treatment of chronic low back pain (cLBP) and to develop a new classification of cLBP based on the pattern of injury. Hypothesis: Surgery may benefit patients with cLBP, and a new classification based on the injury pattern may be of interest. Method: A systematic literature review was performed by searching Medline, the Cochrane Library, the French public health database (Banque de Données en Santé Publique), Science Direct, and the National Guideline Clearinghouse. The main search terms were back pain OR lumbar OR intervertebral disc replacement OR vertebrae OR spinal AND surgery OR surgical OR fusion OR laminectomy OR discectomy. Results: Surgical techniques available for treating cLBP consist of fusion, disc replacement, dynamic stabilisation, and inter-spinous posterior devices. Compared to non-operative management including intensive rehabilitation therapy and cognitive behavioural therapy, fusion is not better in terms of either function (evaluated using the Oswestry Disability Index [ODI]) or pain (level 2). Fusion is better than non-operative management without intensive rehabilitation therapy (level 2). There is no evidence to date that one fusion technique is superior over the others regarding the clinical outcomes (assessed using the ODI). Compared to fusion or multidisciplinary rehabilitation therapy, disc replacement can produce better function and less pain, although the differences are not clinically significant (level 2). The available evidence does not support the use of dynamic stabilisation or interspinous posterior devices to treat cLBP due to degenerative disease (professional consensus within the French Society for Spinal Surgery). The following recommendations can be made: non-operative treatment must be provided for at least 1 year before considering surgery in patients with cLBP due to degenerative disease; patients must be fully informed about alternative treatment options and the risks associated with surgery; standing radiographs must be obtained to assess sagittal spinal alignment and a magnetic resonance imaging scan to determine the mechanism of injury; and, if fusion is performed, the lumbar lordotic curvature must be restored. Discussion: This work establishes the need for a new classification of cLBP based on the presumptive mechanism responsible for the pain. Three categories should be distinguished: non-degenerative cLBP (previously known as symptomatic cLBP), in which the cause of pain is a trauma, spondylolysis, a tumour, an infection, or an inflammatory process; degenerative cLBP (previously known as non-specific cLBP) characterised by variable combinations of degenerative alterations in one or more discs, facet joints, and/or ligaments, with or without regional and/or global alterations in spinal alignment (which must be assessed using specific parameters); and cLBP of unknown mechanism, in which the pain seems to bear no relation to the anatomical abnormalities (and the Fear-Avoidance Beliefs Questionnaire and Hospital Anxiety and Depression Scale may be helpful in this situation). This classification should prove useful in the future for constituting well-defined patient groups, thereby improving the assessment of treatment options.
4. Relevance of Modified Debridement-Irrigation, Antibiotic Therapy and Implant Retention Protocol for the Management of Surgical Site Infections: A Series of 1694
Manet R, Ferry T, Castelain JE, Pardey Bracho G, Freitas-Olim E, Grando J, Barrey CY
J Bone Jt Infect (2018) — Résumé
Introduction: Management of surgical site infections (SSI) after instrumented spinal surgery remains controversial. The debridement-irrigation, antibiotic therapy and implant retention protocol (DAIR protocol) is safe and effective to treat deep SSI occurring within the 3 months after instrumented spinal surgery. Methods: This retrospective study describes the outcomes of patients treated over a period of 42 months for deep SSI after instrumented spinal surgery according to a modified DAIR protocol. Results: Among 1694 instrumented surgical procedures, deep SSI occurred in 46 patients (2.7%): 41 patients (89%) experienced early SSI (< 1 month), 3 (7%) delayed SSI (from 1 to 3 months), and 2 (4%) late SSI (> 3months). A total of 37 patients had a minimum 1 year of follow-up; among these the modified DAIR protocol was effective in 28 patients (76%) and failed (need for new surgery for persistent signs of SSI beyond 7 days) in 9 patients (24%). Early second-look surgery (≤ 7days) for iterative debridement was performed in 3 patients, who were included in the cured group. Among the 9 patients in whom the modified DAIR protocol failed, none had early second-look surgery; 3 (33%) recovered and were cured at 1 year follow-up, and 6 (66%) relapsed. Overall, among patients with SSI and a minimum 1 year follow-up, the modified DAIR protocol led to healing in 31/37 (84%) patients. Conclusions: The present study supports the effectiveness of a modified DAIR protocol in deep SSI occurring within the 3 months after instrumented spinal surgery. An early second-look surgery for iterative debridement could increase the success rate of this treatment.
5. Mortality, complication, and fusion rates of patients with odontoid fracture: the impact of age and comorbidities in 204 cases.
Charles YP, Ntilikina Y, Blondel B, Fuentes S, Allia J, Bronsard N, Lleu M, Nicot B, Challier V, Godard J, Kouyoumdjian P, Lonjon N, Marinho P, Berthiller J, Freitas E, Barrey CY
Arch Orthop Trauma Surg (2019) — Résumé
Purpose The French Society of Spine Surgery (SFCR) conducted a prospective epidemiologic multicenter study. The purpose was to investigate mortality, complication, and fusion rates in patients with odontoid fracture, depending on age, comorbidities, fracture type, and treatment. Methods Out of 204 patients, 60 were ≤ 70 years and 144 were > 70 years. Demographic data, comorbidities, treatment types and complications (general medical, infectious, neurologic, and mechanical), and death were registered within the first year. Fractures were classified according to Anderson-D’Alonzo and Roy-Camille on the initial CT. A 1-year follow-up CT was available in 144 patients to evaluate fracture consolidation. Results Type II and oblique-posterior fractures were the most frequent patterns. The treatment was conservative in 52.5% and surgical in 47.5%. The mortality rate in patients ≤ 70 was 3.3% and 16.7% in patients > 70 years (p = 0.0002). Fracture pattern and treatment type did not influence mortality. General medical complications were significantly more frequent > 70 years (p = 0.021) and after surgical treatment (p = 0.028). Neurologic complications occurred in 0.5%, postoperative infections in 2.0%, and implant-related mechanical complications in 10.3% (associated with pseudarthrosis). Fracture fusion was observed in 93.5% of patients ≤ 70 years and in 62.5% >70 years (p < 0.0001). Pseudarthrosis was present in 31.5% of oblique-posterior fractures and in 24.3% after conservative treatment. Conclusions Age and comorbidities influenced mortality and medical complication rates most regardless of fracture type and treatment choice. Pseudarthrosis represented the main complication, which increased with age. Pseudarthrosis was most frequent in type II and oblique-posterior fractures after conservative treatment.
6. Bone metastases from lung cancer: A paradigm for multidisciplinary onco-rheumatology management
Confavreux CB, Pialat JB, Bellière A, Brevet M, Decroisette C, Tescaru A, Wegrzyn J, Barrey CY, Mornex F, Souquet PJ, Girard N.
Joint Bone Spine (2019) — Résumé
Bone is the third metastatic site after liver and lungs. Bone metastases occur in one out of three lung cancers and are usually of osteolytic aspect. Osteolytic bone metastases are responsible of long bone and vertebral fractures leading to restricted mobility, surgery and medullar compression that severely alter quality of life and that have a huge medico-economic impact. In the recent years, Bone Metastatic Multidisciplinary Tumour Board (BM2TB) have been developed to optimize bone metastases management for each patient in harmony with oncology program. In this review, we will go through all the different aspects of bone metastases management including diagnosis and evaluation (CT scan, Tc 99m-MDP bone scan, 18FDG-PET scan and biopsy for molecular diagnosis), systemic bone treatments (zoledronic acid and denosumab) and local treatments (interventional radiology and radiotherapy). Surgical strategies will be discussed elsewhere. Based on the last 2017-Lung Cancer South East French Guidelines, we present a practical decision tree to help the physicians for decision making in order to reach a personalized locomotor strategy for every patient.
7. A new quasi-invariant parameter characterizing the postural alignment of young asymptomatic adults.
Amabile C, Pillet H, Lafage V, Barrey CY, Vital JM, Skalli W
Eur Spine J (2016) — Résumé
Purpose: Our study aims to describe the postural alignment of young asymptomatic subjects from head to feet from bi-planar standing full-body X-rays, providing database to compare to aging adults. Novelty resides in the inclusion of the head and lower limbs in the erected posture’s analysis. Methods: For 69 young asymptomatic subjects (18-40 years old) 3D reconstructions of the head, spine, pelvis and lower limbs segments were performed from bi-planar full-body X-rays. Usual studied spinal, pelvic and lower limbs’ parameters were computed in 3D, sagittal and frontal planes of the patient. Relationships between these parameters were investigated. Inclinations of different lines were studied to characterize the erected posture. Results: Values found for spinal curvatures, pelvic parameters and lower limbs geometrical parameters agreed with the literature: thoracic kyphosis, lumbar lordosis, pelvic incidence, pelvic tilt and sagittal vertical axis were respectively in average of 26.9° (SD 7.2°), 30.5° (SD 7.5°), 51.0° (SD 9.4°), 11.1° (SD 5.6°) and -8.9 mm (SD 21.6 mm). The angle between the vertical and the line joining the most superior point of dentiform apophyse of C2 (OD) and the center of the bi-coxofemoral axis (HA) was the less variable one (SD 1.6°). Conclusions: This study on 3D postural alignment reports the geometry of the spine, pelvis and lower limbs, of the young asymptomatic adult. The less variable angle is the one of the line OD-HA with the vertical, highlighting the vertical alignment of the head above the pelvis. This study provides a basis for future comparisons when investigating aging populations.
8. Compensatory mechanisms contributing to keep the sagittal balance of the spine
Barrey CY, Roussouly P, Le Huec JC, D’Acunzi G, Perrin G
Eur Spine J (2013) — Résumé
Introduction: Aging spine is characterized by facet joints arthritis, degenerative disc disease, bone remodeling and atrophy of extensor muscles resulting in a progressive kyphosis of the lumbar spine. Objective: The aim of this paper is to describe the different compensatory mechanisms for patients with severe degenerative lumbar spine. Material and methods: According to the severity of the imbalance, three stages are observed: balanced, balanced with compensatory mechanisms and imbalanced. For the two last stages, the compensatory mechanisms permit to limit the consequences of loss of lumbar lordosis on global sagittal alignment and therefore contribute to keep the sagittal balance of the spine. Results: The basic concept is to extend adjacent segments of the kyphotic spine allowing for compensation of the sagittal unbalance but potentially inducing adverse effects. Conclusion: Finally, we propose a three-step algorithm to analyze the global balance status and take into consideration the presence of the compensatory mechanisms in the spinal, pelvic and lower limb areas.
9. Cervical disc prosthesis versus arthrodesis using one-level, hybrid and two-level constructs: an in vitro investigation
Barrey CY, Campana S, Persohn S, Perrin G, Skalli W
Eur Spine J (2012) — Résumé
Introduction The purpose of this experimental study was to analyse cervical spine kinematics after 1-level and 2-level total disc replacement (TDR) and compare them with those after anterior cervical arthrodesis (ACA) and hybrid construct. Kinematics and intradiscal pressures were also investigated at adjacent levels. Methods Twelve human cadaveric spines were evaluated in different testing conditions: intact, 1 and 2-level TDR (Discocerv™, Scient’x/Alphatec), 1 and 2-level ACA, and hybrid construct. All tests were performed under load control protocol by applying pure moments loading of 2 N m in flexion/extension (FE), axial rotation (AR) and lateral bending (LB). Results Reduction of ROM after 1-level TDR was only significant in LB. Implantation of additional TDR resulted in significant decrease of ROM in AR at index level. A second TDR did not affect kinematics of the previously implanted TDR in FE, AR and LB. One and 2-level arthrodesis caused significant decrease of ROM in FE, AR and LB at the index levels. No significant changes in ROM were observed at adjacent levels except for 1-level arthrodesis in FE and hybrid construct in AR. When analysis was done under the displacement-control concept, we found that 1 and 2-constructs increased adjacent levels contribution to global ROMC3–C7 during FE and that IDP at superior adjacent level increased by a factor of 6.7 and 2.3 for 2-level arthrodesis and hybrid constructs, respectively. Conclusion Although 1- and 2-level TDR restored only partially native kinematics of the cervical spine, these constructs generated better biomechanical conditions than arthrodesis at adjacent levels limiting contribution of these segments to global ROM and reducing the amount of their internal stresses.
10. Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases
Barrey CY, Jund J, Noseda O, Roussouly P
Eur Spine J (2007) — Résumé
Retrospective analysis of the spino-pelvic alignment in a population of 85 patients with a lumbar degenerative disease. Several previous publications reported the analysis of spino-pelvic alignment in the normal and low back pain population. Data suggested that patients with lumbar diseases have variations of sagittal alignment such as less distal lordosis, more proximal lumbar lordosis and a more vertical sacrum. Nevertheless most of these variations have been reported without reference to the pelvis shape which is well-known to strongly influence spino-pelvic alignment. The objective of this study was to analyse spino-pelvic parameters, including pelvis shape, in a population of 85 patients with a lumbar degenerative disease and compare these patients with a control group of normal volunteers. We analysed three different lumbar degenerative diseases: disc herniation (DH), n = 25; degenerative disc disease (DDD), n = 32; degenerative spondylolisthesis (DSPL), n = 28. Spino-pelvic alignment was analysed pre-operatively on full spine radiographs. Spino-pelvic parameters were measured as following: pelvic incidence, sacral slope, pelvic tilt, lumbar lordosis, thoracic kyphosis, spino-sacral angle and positioning of C7 plumb line. For each group of patients the sagittal profile was compared with a control population of 154 asymptomatic adults that was the subject of a previous study. In order to understand variations of spino-pelvic parameters in the patients’ population a stratification (matching) according to the pelvic incidence was done between the control group and each group of patients. Concerning first the pelvis shape, patients with DH and those with DDD demonstrated to have a mean pelvic incidence equal to 49.8 degrees and 51.6 degrees, respectively, versus 52 degrees for the control group (no significant difference). Only young patients, less than 45 years old, with a disc disease (DH or DDD) demonstrated to have a pelvic incidence significantly lower (48.3 degrees) than the control group, P < 0.05. On the contrary, in the DSPL group the pelvic incidence was significantly greater (60 degrees) than the control group (52 degrees), P < 0.0005. Secondly the three groups of patients were characterized by significant variations in spino-pelvic alignment: anterior translation of the C7 plumb line (P < 0.005 for DH, P < 0.05 for DDD and P < 0.05 for DSPL); loss of lumbar lordosis after matching according to pelvic incidence (P < 0.0005 for DH, DDD and DSPL); decrease of sacral slope after matching according to pelvic incidence (P = 0.001 for DH, P < 0.0005 for DDD and P < 0.0005 for DSPL). Measurement of the pelvic incidence and matching according to this parameter between each group of patients and the control group permitted to understand variations of spino-pelvic parameters in a population of patients.